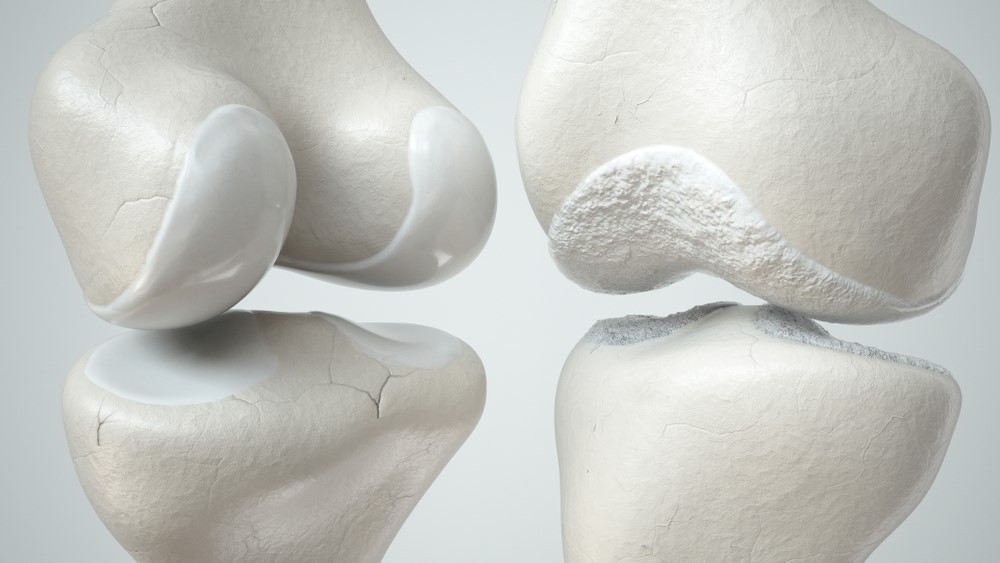
The bones in our joints are typically covered in hyaline cartilage, a type of smooth cartilage that allows for painless and fluid movement of the joints. Cartilage also serves as a shock absorber for our joints when we do weight-bearing activities. Osteochondral lesions are injuries to the cartilage that can be caused by trauma or overuse of the joint. The cartilage can be eroded, crushed or damaged, and less commonly can form cysts. This may cause swelling, stiffness and pain when walking.
The difference between osteochondral injuries and arthritis is that the former is usually a localised injury and relatively small in size, whereas arthritis typically involves large areas of cartilage degeneration. Because osteochondral injuries usually comprise small areas of cartilage injury (in the early stages), this condition can be effectively treated with arthroscopic “keyhole” or minimally invasive surgical (MIS) techniques when dealt with early.
Osteochondral injuries can occur in any joint, but most frequently affects the knee and ankle joints. In this article, we will be covering common causes of osteochondral injuries, the associated symptoms, diagnosis of these lesions, as well as the treatment options available.
Generally, osteochondral lesions arise from injury to the joint in the form of repetitive strain or direct trauma, such as a sprain.
People who engage in vigorous or high-energy sports such as football, rugby or running are at a higher risk of sustaining an osteochondral injury in the knee joint.
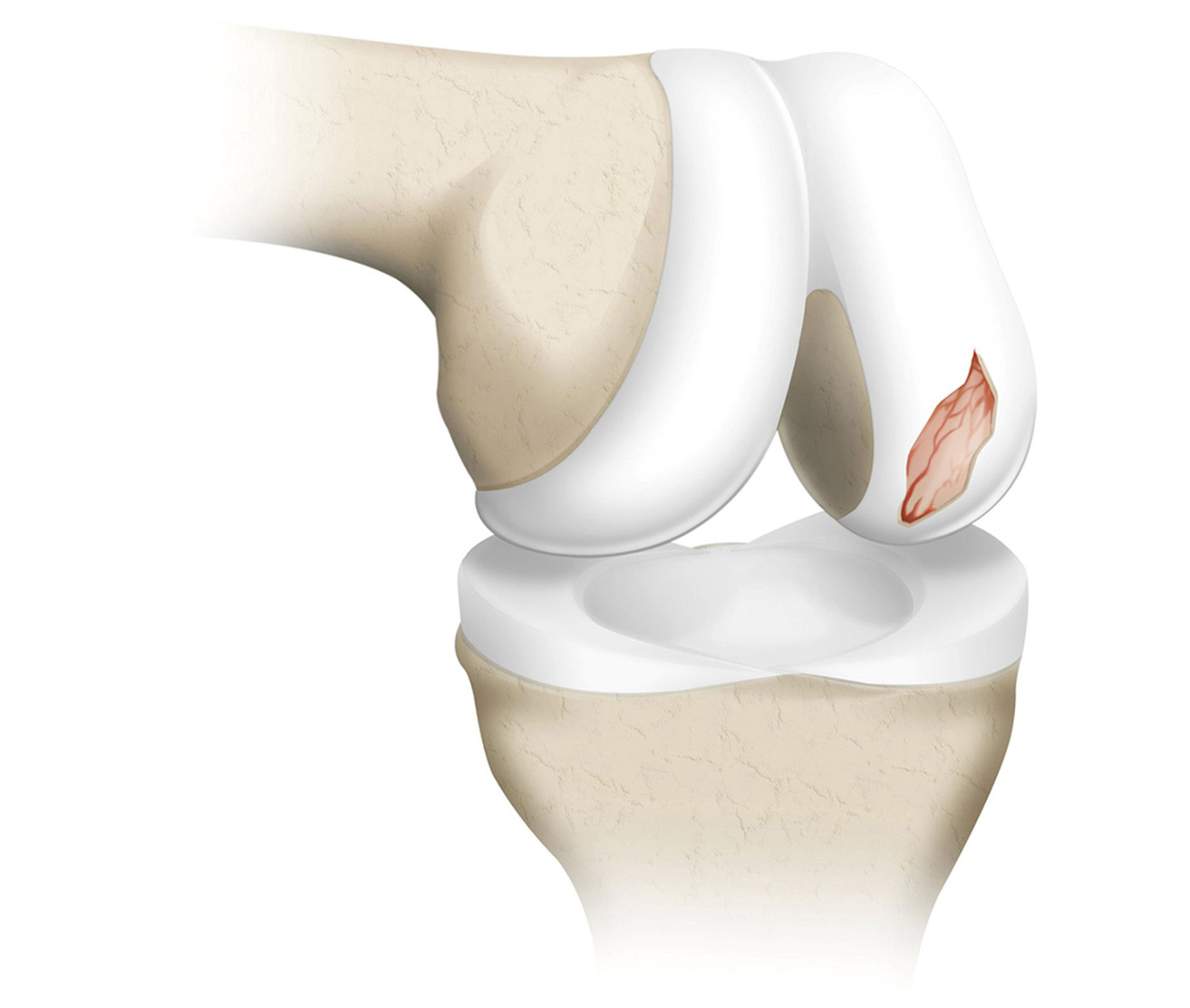
High-impact or twisting knee injuries are at a particularly high risk of causing permanent localized damage to the cartilage, as they impart direct shearing forces to the knee cartilage, resulting in osteochondral lesions.
Knee cartilage serves as a shock absorber when moving and prevents your knee bones (femur & tibia) from rubbing directly against each other. Hence, osteochondral injuries will cause significant pain when engaging in simple activities like walking, stair climbing and cycling, and will also cause the knee joint to be worn out more quickly, leading to osteoarthritis eventually if left untreated.
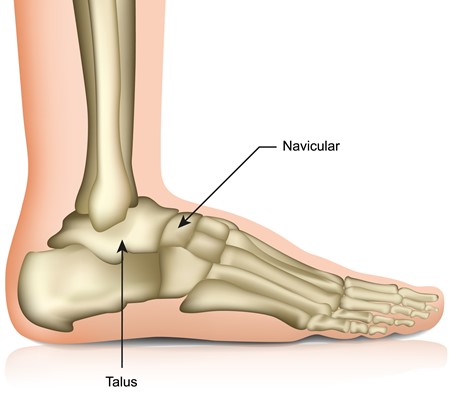
Ankle sprains are the most common cause of ankle osteochondral lesions, often causing crushing or shearing of the ankle joint cartilage. Such injuries most frequently occur at the talus, one of the weight-bearing bones in the ankle joint (see diagram below, in red).
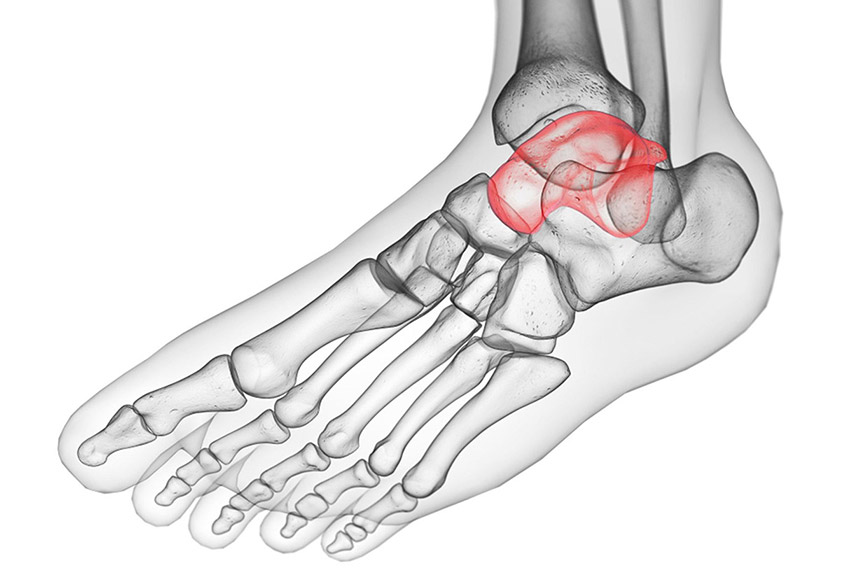
This mechanism of injury leads to a detachment or defect in the cartilage, subsequently leading to pain in the foot or ankle when bearing weight. Additionally, since the ankle joint controls the ability of the foot to move up (dorsiflex) and down (plantarflex) when walking, this injury will impair one’s ability to walk normally without experiencing pain or stiffness. Sporting activities are typically severely curtailed by the pain as well.
If you have an osteochondral injury, below are some of the more common symptoms that you may experience in the affected joint:
- Pain – If you experience pain when engaging in weight-bearing activities that you were previously able to do, or if there is a new onset of pain after a recent joint injury, you should seek medical attention.
- Decreased range of motion & swelling – As with any injury, there is often swelling as the body tries to heal the affected area. The combination of swelling and pain may lead to a decreased range of motion of the injured joint.
- Locking of the joint – If your joint frequently ‘locks’ or experiences a catching sensation after a prolonged period of rest, it may mean that a large area of cartilage may have detached, and this cartilage fragment may have become stuck in the joint.
- Swelling – This indicates underlying inflammation and persistent injury in the joint, and may impair your quality of life.
- Instability of the joint – The pain and injured cartilage both contribute to a subjective sensation of instability in the joint; also, joint instability can lead to osteochondral injuries, and is often an underlying risk factor for osteochondral injuries.
When you attend your consultation, your doctor will take a detailed history from you, asking specifically about any recent trauma or old sports injuries, and will assess how this injury has affected your function. The doctor will then go on to examine the affected joint, taking particular note of areas of tenderness, and assessing the joint for signs of instability and co-existing injuries.
After the clinical examination, X-rays will typically be taken to look for signs of osteochondral injuries and joint deformities. Additional radiological imaging such as MRI and/or CT scans are often performed to confirm the diagnosis and determine the site, size and severity of the osteochondral lesion. MRI scans can also look for co-existing injuries such as ligament, muscle tendon, and meniscal injuries. This constellation of information will help your surgeon in deciding if surgery is necessary, and if so, provide invaluable imagery to aid pre-operative planning.
There are various treatment options that your doctor will advise you on, varying according to the severity of your symptoms and desired level of activity.
Conservative methods include painkillers, physiotherapy, heat therapy, and resting the affected joint. Reducing the amount of high-impact sports or weight-bearing activities, wearing a brace and taping the joint may help as well.
If these non-surgical methods fail to relieve your pain or restore your function adequately, surgery is typically the next step in relieving your symptoms. There are two main options for surgery – traditional open surgery and arthroscopic “keyhole” surgery.
“Keyhole” surgery, also known as arthroscopy, is the most frequently used treatment option for dealing with osteochondral injuries, as it is much less invasive and has a lower risk of complications (infection, bleeding, wound breakdown and soft tissue injury) than open surgery. Indeed, arthroscopic surgery has now become the mainstay for treating osteochondral injuries in both the knee and ankle after failure of conservative measures.
As its name suggests, this efficient and minimally-invasive surgical (MIS) procedure involves a subcentimetre “keyhole” stab incision being made to provide access the affected joint. Then, a tiny specialised camera is inserted through this small “keyhole” incision to look inside the joint and allow the surgeon to visually confirm the site and size of the cartilage damage. The surgeon will also inspect the rest of the knee or ankle joint for co-existing injuries to other structures.
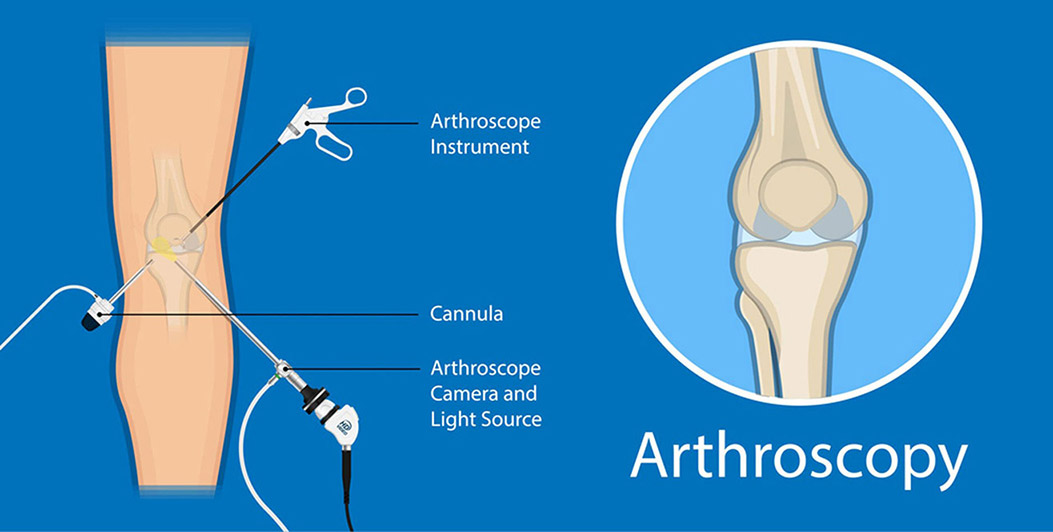
Once the osteochondral lesion has been identified on camera, repair of the affected cartilage and / or removal of loose cartilage fragments is performed arthroscopically by inserting specialised instruments through a second “keyhole” incision.
To stimulate healing and repair of the osteochondral injury, your surgeon may offer a procedure called microfracture, which is done via the abovementioned arthroscopic “keyhole” surgery. During the microfracture procedure, a small instrument called an “awl” is inserted into the second “keyhole” incision, under direct camera visualization, and is used to make multiple tiny drill holes in the area of bone directly underlying the osteochondral lesion. These tiny drill holes (“microfractures”) permit stem cells from the bone marrow to enter the zone of osteochondral injury, which promotes repair and regeneration of the injured cartilage.
Another surgical option, apart from microfracture, is minimally invasive surgical (MIS) drilling of the osteochondral lesion. In this MIS drilling method, arthroscopy is not required and the affected joint does not have to be accessed directly (unlike in the arthroscopic microfracture technique). Instead, by using X-ray imaging for guidance, a small drill bit can be introduced through a single subcentimetre “keyhole” incision (instead of the two incisions used in arthroscopy). This is then used to drill the osteochondral lesion, using X-ray imaging to ensure the drill bit engages the lesion accurately, and hence, permitting stem cells from the bone marrow to enter the zone of osteochondral injury and promoting repair and regeneration of the injured cartilage.
The advantages of this MIS drilling technique are that it is even more minimally invasive than microfracture surgery, avoids the need to violate the knee or ankle joint directly, and utilises only a single small stab incision instead of two. The advantage of arthroscopic microfracture surgery is that it allows direct inspection of the knee or ankle joint, and provides the opportunity to remove loose bodies and address co-existing joint injuries during the same surgery, if any.
Regardless of whether you undergoing arthroscopic microfracture or MIS drilling of the osteochondral injury, your surgeon will typically keep you on crutches to avoid putting weight on the affected joint for 3 to 6 weeks, and this allows the injured cartilage to be healed with the stem cells. Once healing is complete, you can expect the knee or ankle pain to improve significantly, and rehabilitation can commence, focusing on improving the strength and range of motion in the joint to allow you to return to daily activities and sports. Your physiotherapist will also teach you various methods to strengthen your joint and surrounding muscles to prevent future injuries.

Osteochondral injuries of the knee and ankle joints are typically permanent if left untreated, and the injured cartilage does not regenerate spontaneously, resulting in chronic pain and recurrent swelling. Furthermore, there may be broken and loose fragments in the joint that can cause locking symptoms which require surgery for removal.
It is advisable to seek consultation if you have symptoms such as persistent pain, locking, stiffness or swelling in your knee or ankle that is affecting your ability to walk or participate in sports. Early diagnosis and prompt treatment typically results in excellent pain relief and return to activity, and can help to prevent osteoarthritis of the knee or ankle from setting in.
Additionally, with the advent of arthroscopic “keyhole” and minimally invasive surgical (MIS) techniques, osteochondral lesions of both the knee and ankle can now be very effectively treated, with minimal post-operative pain, rapid recovery and very low complication rates. Visit your surgeon promptly if you suspect that you have suffered an osteochondral injury, and give your joint the best chance for a swift recovery.
In subtalar, talonavicular and/or calcaneocuboid fusion surgery (also called triple fusion or triple arthrodesis), the areas of damaged bone and cartilage in these joints are carefully removed. After restoring the correct shape of the foot, the subtalar, talonavicular and/or calcaneocuboid joints are held in place with metal screws or plates. Similar to ankle fusion (described above), the bones in these joints will fuse together, resulting in greater stability and reliable pain relief.
When done using the “keyhole” technique, arthroscopic triple fusion has much lower skin complications and infections that are problematic with open surgery. Arthroscopic triple arthrodesis has the additional benefits of much less pain, more rapid recovery, earlier discharge home (often within a day), and better fusion rates. Patients typically report better and faster return to activity and work following arthroscopic triple fusion.
Lastly, arthritis can also develop in the joints in the middle (midfoot) and front (forefoot) of the foot. These conditions can initially be treated with analgesics, footwear and activity modification. When severe, however, OA of the midfoot and forefoot can be effectively treated with surgical fusion of the affected joints, typically with excellent results.
Although OA cannot be reversed, the outlook is very positive with treatment. Chronic joint pain, stiffness and deformity should not be ignored, particularly in the weight-bearing joints of the lower limb that are crucial to your mobility and daily activities. Do seek early consultation with your doctor if you have any concerns. The sooner treatment is administered, the better the outcomes, and the sooner your quality of life can be improved.

