Tendons are thick bands of connective tissue that link muscle and bone. Tendon injuries, commonly known as tendinitis or tendinopathy, occur when the tendons get inflamed or torn. Most tendon injuries occur in the shoulders, elbows, wrists, knees, and heels, where there is a greater amount of wear and tear. However, a tendon injury can actually occur in any of the tendons.

Tendon injuries can be caused by trauma, but are more likely to be the result of overuse or simple wear and tear over time. Repetitive motions can put stress on the tendons and cause them to weaken or even tear. An overstretched or torn tendon is often called a strain.
A weak tendon is more prone to injury and can be caused by an inactive lifestyle, previous injury, or genetic conditions.
Age is also a factor to consider, as tendons tend to become less flexible — and thus, more susceptible to injury — over time.


Most tendon injuries involve inflammation and minor tears. These only require rest, medication, and maybe physical therapy in order to heal.
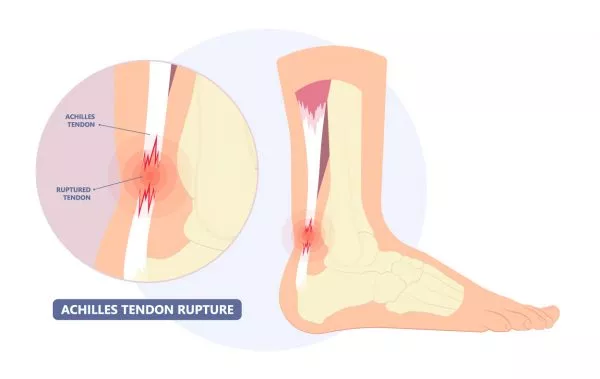
However, severe tendon injuries that lead to ruptures may require surgical treatment as the body cannot correctly heal tendon ruptures on its own.
Minor tendon injuries can usually be treated at home using the RICE method. This involves:
If the injury is still causing you pain after 2 weeks of RICE treatment, it might be time to visit a medical professional for further treatment. This might take the form of physical therapy or, in worst-case scenarios, tendon repair surgery.
During tendon repair surgery, your surgeon will make a small incision to access the injured tendon, and sew the torn ends of the tendon back together. After the surgery, you will be fitted with a splint or a cast. The healing process can take up to 12 weeks, and usually involves physical therapy as well.
Although tendon injuries tend to be minor, if left untreated, they can easily worsen into a more serious problem, such as a ruptured tendon. This can result in pain, instability, arthritis, or even disability in the affected limb.
If you are experiencing minor pain and swelling, please treat your injury at home with the aforementioned RICE treatment. For more severe issues, please approach a medical professional for treatment.

Your doctor will first ask about your symptoms and perform a physical examination. You can also expect questions regarding your general health, medical history, and lifestyle. If your injury is related to a certain sport or activity, you may be asked to perform this activity under your doctor’s observation.
If your symptoms are severe or have persisted over a prolonged period of time, your doctor may order an X-ray or other imaging tests to properly diagnose the problem. If necessary, surgical options may be discussed as well.
“Keyhole” surgery, also known as arthroscopy, is the most frequently used treatment option for dealing with osteochondral injuries, as it is much less invasive and has a lower risk of complications (infection, bleeding, wound breakdown and soft tissue injury) than open surgery. Indeed, arthroscopic surgery has now become the mainstay for treating osteochondral injuries in both the knee and ankle after failure of conservative measures.
As its name suggests, this efficient and minimally-invasive surgical (MIS) procedure involves a subcentimetre “keyhole” stab incision being made to provide access the affected joint. Then, a tiny specialised camera is inserted through this small “keyhole” incision to look inside the joint and allow the surgeon to visually confirm the site and size of the cartilage damage. The surgeon will also inspect the rest of the knee or ankle joint for co-existing injuries to other structures.
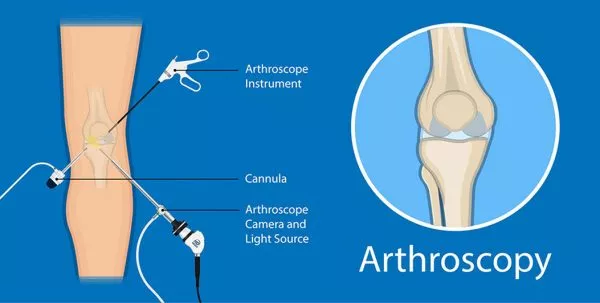
Once the osteochondral lesion has been identified on camera, repair of the affected cartilage and / or removal of loose cartilage fragments is performed arthroscopically by inserting specialised instruments through a second “keyhole” incision.
To stimulate healing and repair of the osteochondral injury, your surgeon may offer a procedure called microfracture, which is done via the abovementioned arthroscopic “keyhole” surgery. During the microfracture procedure, a small instrument called an “awl” is inserted into the second “keyhole” incision, under direct camera visualization, and is used to make multiple tiny drill holes in the area of bone directly underlying the osteochondral lesion. These tiny drill holes (“microfractures”) permit stem cells from the bone marrow to enter the zone of osteochondral injury, which promotes repair and regeneration of the injured cartilage.
Another surgical option, apart from microfracture, is minimally invasive surgical (MIS) drilling of the osteochondral lesion. In this MIS drilling method, arthroscopy is not required and the affected joint does not have to be accessed directly (unlike in the arthroscopic microfracture technique). Instead, by using X-ray imaging for guidance, a small drill bit can be introduced through a single subcentimetre “keyhole” incision (instead of the two incisions used in arthroscopy). This is then used to drill the osteochondral lesion, using X-ray imaging to ensure the drill bit engages the lesion accurately, and hence, permitting stem cells from the bone marrow to enter the zone of osteochondral injury and promoting repair and regeneration of the injured cartilage.
The advantages of this MIS drilling technique are that it is even more minimally invasive than microfracture surgery, avoids the need to violate the knee or ankle joint directly, and utilises only a single small stab incision instead of two. The advantage of arthroscopic microfracture surgery is that it allows direct inspection of the knee or ankle joint, and provides the opportunity to remove loose bodies and address co-existing joint injuries during the same surgery, if any.
Regardless of whether you undergoing arthroscopic microfracture or MIS drilling of the osteochondral injury, your surgeon will typically keep you on crutches to avoid putting weight on the affected joint for 3 to 6 weeks, and this allows the injured cartilage to be healed with the stem cells. Once healing is complete, you can expect the knee or ankle pain to improve significantly, and rehabilitation can commence, focusing on improving the strength and range of motion in the joint to allow you to return to daily activities and sports. Your physiotherapist will also teach you various methods to strengthen your joint and surrounding muscles to prevent future injuries.


If surgical treatment is necessary, you can expect the resultant healing process to take up to 12 weeks.
Immediately after the surgery, you will be fitted with a splint or a cast. During this time, some pain and swelling are to be expected. It is important to rest and avoid the use of the affected limb during this phase of the recovery process.
After 3 to 5 days, the swelling will go down and you will begin to have a limited range of motion in the affected area. Physical therapy under a medical professional will be needed over a prolonged period of time in order to safely regain full use of the affected area.
If there is too much resulting scar tissue after the healing period is over, you may be required to undergo another surgery to remove this scar tissue, as it can affect mobility as well.

Tendon injuries are common and are only a cause for worry in serious cases. Often, they can be treated simply with rest. Preventative measures can also be taken to reduce the likelihood of tendon injury. These include taking short rests during prolonged periods of work or exercise, stretching, using ergonomic equipment, or strengthening the muscles around the joints.
If you are experiencing persistent pain or swelling in the tendons that do not respond to medication or rest, please do not hesitate to approach a medical professional for assistance as these may be a sign of a more serious issue.
Our friendly team is here to serve you. For urgent enquiries and appointment requests, please call or WhatsApp us directly.
