It doesn’t always arrive as a dramatic injury. At first, the knee still works. You can walk, you can function, and you can get through most days. Yet the problem becomes obvious when your knee has to take real load. Stairs, downhill walking, longer distances, and standing up after rest start to feel less smooth, as if one side of the joint has become more sensitive and less forgiving. Over time, it can start to feel like the issue is not the whole knee, but a specific area that keeps taking the strain.
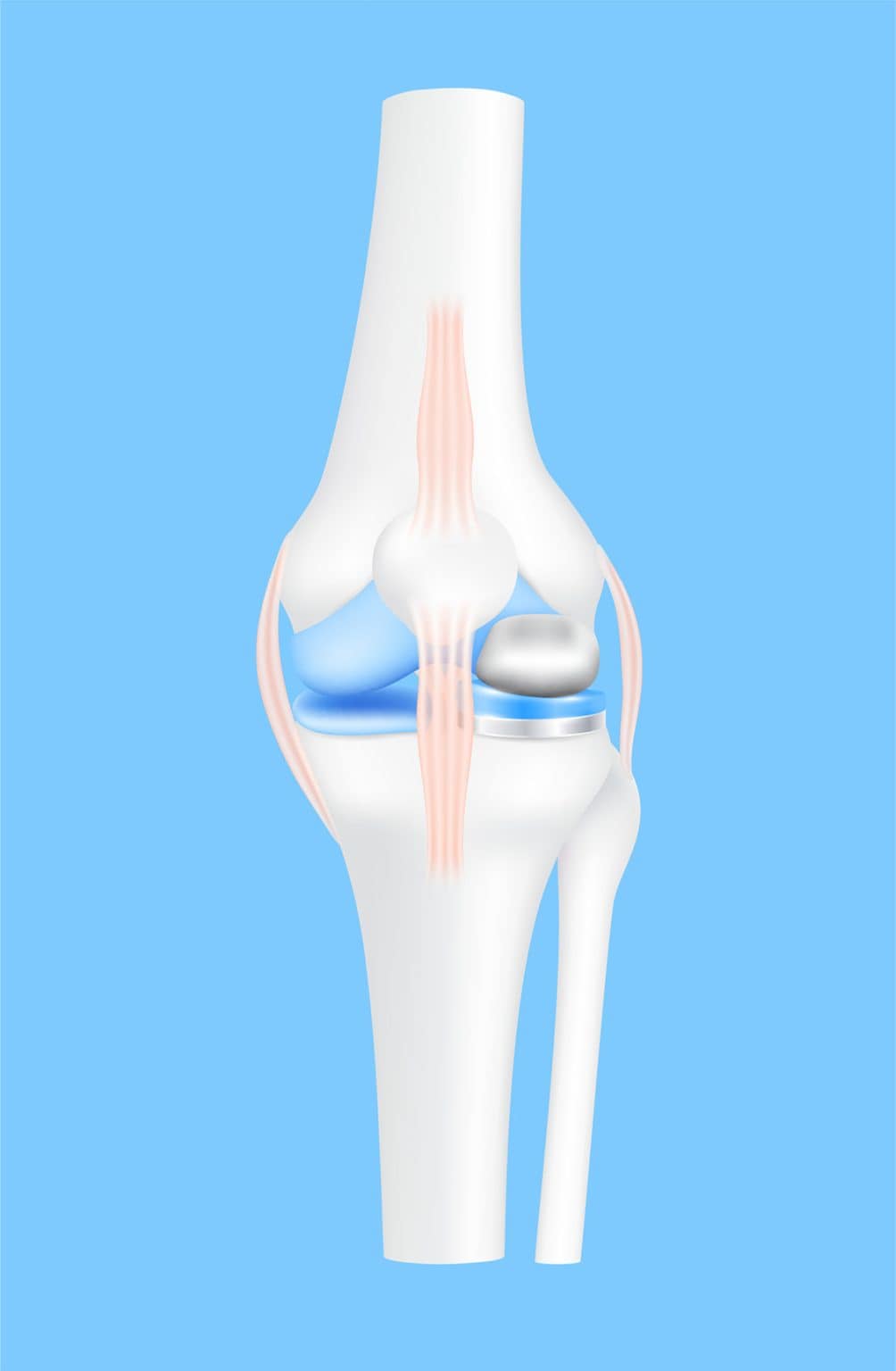
Once pain and stiffness keep showing up in the same manner, the next step is working out where the wear is coming from, and how much of the knee is actually involved. When damage is limited to one compartment, a partial knee replacement (PKR) might be considered instead of replacing the entire joint. Also known as unicompartmental knee arthroplasty (UKA), it’s designed to replace only the affected area of the knee while preserving the healthier parts around it. For some patients, this is also when a second opinion becomes important, especially if a total knee replacement (TKR) has been suggested and they want to confirm whether a partial approach is still possible. Since suitability depends on where the damage lies and what structures are still functioning well, the next step is identifying which knee conditions can be considered for PKR/UKA.

Once pain and stiffness keep showing up in the same manner, the next step is working out where the wear is coming from, and how much of the knee is actually involved. When damage is limited to one compartment, a partial knee replacement (PKR) might be considered instead of replacing the entire joint. Also known as unicompartmental knee arthroplasty (UKA), it’s designed to replace only the affected area of the knee while preserving the healthier parts around it. For some patients, this is also when a second opinion becomes important, especially if a total knee replacement (TKR) has been suggested and they want to confirm whether a partial approach is still possible. Since suitability depends on where the damage lies and what structures are still functioning well, the next step is identifying which knee conditions can be considered for PKR/UKA.
Since partial knee replacement is designed for wear that’s limited to one compartment of the knee, suitability depends on where the damage is concentrated, and whether the rest of the joint still functions well. It’s most often considered when changes are confined to a single tibiofemoral compartment, either the medial (inner) or lateral (outer) side of the knee, with preserved stability and alignment. In comparison, it’s generally not advisable when damage affects more than one compartment, or when significant ligament instability is present. Situations where partial knee replacement is considered include:
Note: Unicompartmental knee arthroplasty (UKA) refers to a partial knee replacement that treats a single tibiofemoral compartment, with “unicompartmental” describing damage that’s limited to one compartment. When arthritis is isolated to the kneecap joint instead, a patellofemoral arthroplasty (PFA) might be considered as a different type of partial knee replacement.

If you’ve been searching for info on “partial vs full knee replacement” online, it’s most likely after a consult with a specialist where total knee replacement is presented as the best option for your knee, and you’re trying to confirm whether a full replacement is necessary, or whether a partial knee replacement procedure can be considered instead. Since knee replacement surgery is a significant decision, it’s normal to want clarity when total knee replacement is suggested.
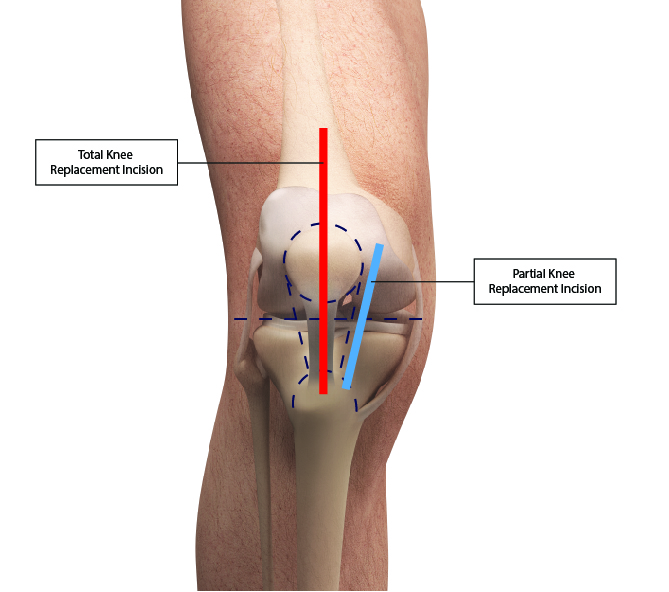
In Singapore, the two main orthopaedic surgical options are partial and total knee replacement, and the choice usually depends on whether the damage is confined to one compartment or affects multiple areas of the knee. Because these procedures involve different surgical scopes, the general recovery timeline, hospital stay, and overall costs can differ as well. Key differences between the two include:
For suitable patients, partial knee replacement is recommended when the problem is clearly localised to one compartment and the rest of the knee is still worth preserving. And because the surgery changes less of the knee overall, recovery often feels less overwhelming, since patients are usually rehabilitating one compartment rather than adapting to a total joint replacement. Benefits that are commonly associated with partial knee replacement include:


Even when a partial knee replacement is recommended, it’s still a form of knee replacement surgery, which means it comes with risks like any other surgical procedure. And because this orthopaedic procedure only works well when damage is localised to one compartment, the outcome depends on careful selection, precise surgical technique, and how well the knee heals during recovery. Potential risks and complications can include:
Note: Beyond these general surgical risks, the main limitation of partial knee replacement is that it only treats one compartment. And if arthritis progresses in other parts of the knee, a conversion to a total replacement of the knee would be required.
The Oxford Partial Knee System was developed to address two challenges that affected older partial knee replacement designs: implant loosening and plastic insert wear. In traditional fixed bearing designs, the knee’s twisting motion is repeatedly channelled through one fixed contact surface during everyday activity. As the knee bends and rotates, this twisting load is repeatedly transferred into the cement that holds the implant to bone, which can strain the bond and reduce long term fixation strength.
For this reason, the Oxford Partial Knee System uses a mobile bearing design, where controlled movement is built into how the implant works. Instead of locking the plastic insert in place on the tibial base, the insert is designed to float and move freely on top of it as the knee bends and rotates. This allows everyday twisting forces to be absorbed through the insert’s mobility, rather than being repeatedly transferred into the cemented fixation. And since the insert surface is shaped to match the curve of the femoral component closely, load is spread across a broader area instead of being concentrated in one spot. This is made possible through the implant’s key components working together.
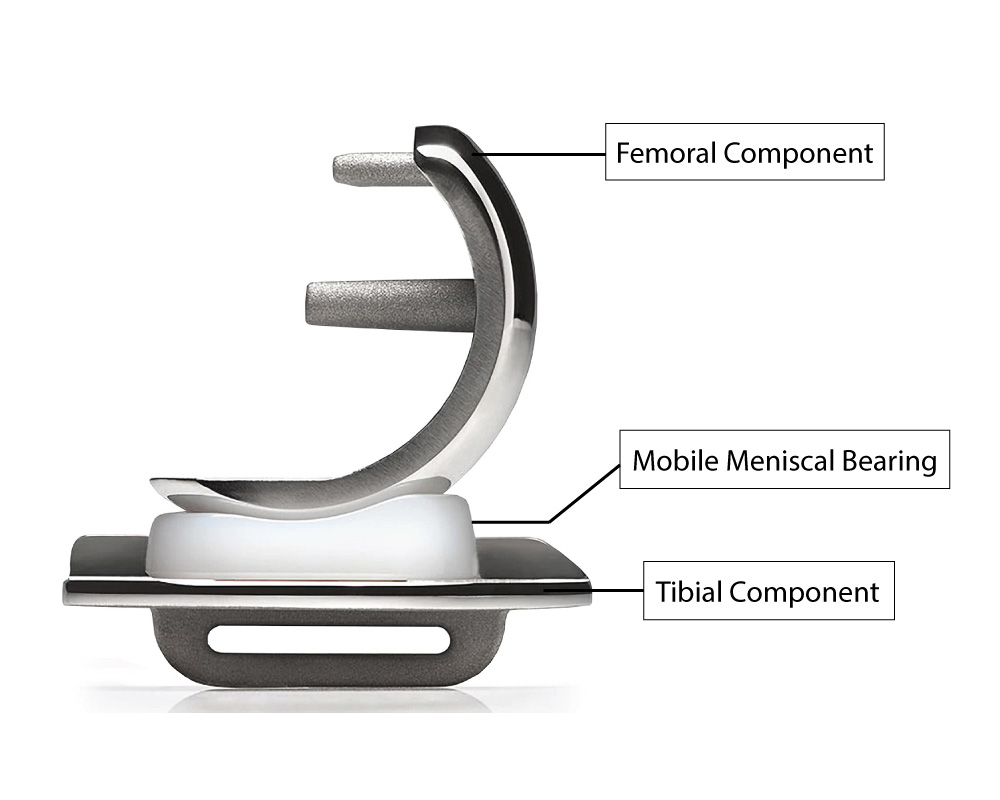
The Oxford Partial Knee System consists of three components that work together inside the treated knee compartment:
Rather than acting as separate parts, these components are designed to work together as the knee bends, straightens, and rotates under load. And this design is what supports the three key things patients tend to care about most:
If you’re preparing for a partial knee replacement surgery, it’s normal to have questions that don’t always come up during consultation with the doctor, such as what happens in the operating room, what the first phase of recovery is about, and what rehabilitation is meant to focus on in the early stages. To help you feel more prepared, the process below explains what typically happens before surgery, during the procedure, and in the early phase of recovery thereafter.
In the lead up to the operation, your specialist will go through a final round of assessment and planning with you. This usually includes revisiting your symptoms, reviewing the most recent X-rays of the knee, and in some cases other imaging such as MRI or CT scans when needed. These help confirm which part of the joint will be treated and guide how the implant should be best positioned, so the surgical plan is tailored to your knee.
You will also have a pre-operative medical review so the care team understands your general health, existing conditions, and medications. This is often when anaesthesia options and hospital arrangements are discussed, questions about risks and recovery are addressed, and initial plans are made for physiotherapy and support at home, giving you a clearer picture of how the first phase after surgery will be managed.
At the start of the operation, the anaesthesia plan is carried out according to the joint decision made earlier between you, your specialist, and the anaesthesia team. This is usually a general anaesthetic that puts you fully to sleep, or a regional technique such as a spinal anaesthetic that numbs the lower body while medication is given to help you stay relaxed or sleepy throughout the surgery.
Once the anaesthesia has taken effect, the orthopaedic surgeon makes a small incision over the affected side of the knee and uses a minimally invasive approach to reach the damaged compartment without fully opening the joint. Damaged bone and cartilage are then removed in a controlled way to prepare the surfaces for resurfacing, and the implant components are then placed to restore the treated compartment. The knee is then moved through its range to check that positioning and function are as intended, and once this has been confirmed, the wound is closed to complete the partial knee replacement procedure.
After the partial knee replacement surgery, you’ll be moved to a recovery room or ward, where the care team monitors you as the anaesthesia wears off. During this early phase, the focus is on pain control, blood circulation in the legs, and gentle movement within your comfort level, so the knee and surrounding muscles aren’t stiffening up more than necessary.
As you become more settled, nurses and therapists might gradually introduce simple assisted movements in line with your specialist’s advice. For many this can include supported sitting or standing when it is safe to do so, before progressing further. As you stabilise, your specialist will also outline the next phase of recovery, including physiotherapy, walking progression, and follow up reviews, so you know what to expect once the formal rehabilitation process begins.


Rehabilitation after partial knee replacement surgery focuses on rebuilding strength and confidence around the joint, so the knee can move smoothly again in daily life. Because recovery speed differs from person to person, your plan is usually adjusted to how your knee is responding, rather than forcing a timeline that doesn’t fit. In the initial stage, physiotherapy often starts with gentle bending and straightening, basic strength work for the thigh and hip muscles, and short walks with a frame, crutch, or cane if you need support. Your specialist and physiotherapist will also guide you on pacing, including how long to stay on your feet at a stretch, when to rest and elevate the leg, and how to spread activity through the day so the knee keeps improving without being pushed into flare ups.
As control improves, walking and daily routines become the main way progress is built. Step by step, you might increase walking distance, be less reliant on walking aids when it’s safe to do so, and return to regular tasks in shorter blocks instead of one long effort. When the knee tolerates more, lower impact options such as gentle indoor cycling or pool-based exercises can be added before anything more demanding, while twisting, deep bending, and impact are usually delayed until strength, balance, and control have improved further.
If you’re exploring partial knee replacement surgery, then you’re likely looking for clarity on whether the damage is still confined to one compartment, or whether more of the joint is involved. Since this isn’t always clear from symptoms alone, an assessment is important to confirm whether a partial knee replacement procedure is still a good fit for your knee. This matters because a partial approach only works well when wear is truly localised and the knee remains stable enough to preserve the healthier structures around it.
At Oxford Orthopaedics, the assessment begins by examining how the knee moves, bears weight, and holds stability through everyday positions and motion. These findings then guide how your X-rays and any other imaging are interpreted, helping confirm whether the joint changes are truly confined to one compartment. Dr James Wee then explains what the findings mean for function and day to day movement, and whether partial knee replacement surgery is the best option for your knee. He will also walk you through what the procedure involves, what recovery typically looks like, and what the next steps should look like, so you can move forward with more confidence. To speak to our specialist, please contact the clinic to arrange a consultation.

Partial knee replacement surgery is usually considered when damage is limited to one compartment, either the inner or outer side of the knee. To be suitable for this procedure, the rest of the joint needs to be healthy enough for preservation. As such, your orthopaedics specialist will first check how stable the knee is under load, whether the key ligaments are still functioning well, and whether your movement is reasonably maintained. In many cases, it’s discussed when pain and stiffness keep returning despite physiotherapy, activity changes, medication, or injections.
Your specialist will first check to see if your symptoms fit a single compartment problem, rather than wear across the whole knee. This starts with a physical examination to assess where the pain is coming from, how stable the knee feels under load, and whether alignment is still reasonably maintained. X-rays are then reviewed to confirm which compartment is affected and how localised the damage is. If more clarity is needed, imaging such as MRI or CT scans can help assess cartilage damage and ligament health. From there, the decision comes down to whether the rest of the joint can still be preserved for a partial approach.
If you’re looking up “partial vs full knee replacement” online, it’s most likely due to the fact that a total knee replacement procedure has been suggested and you’re trying to confirm whether it’s even necessary. The clearest difference is scope. A partial knee replacement treats one damaged compartment, while a total knee replacement replaces most or all of the joint surfaces. Because the partial approach is more targeted, more natural bone and supporting structures are preserved, including key ligaments when intact. For suitable patients, this usually translates into a knee that feels more natural during daily movement, as more of the original joint mechanics are preserved.
The Oxford Partial Knee System uses a mobile bearing design, which means the plastic insert is able to move as the knee bends and rotates. Because of this, twisting forces are absorbed through controlled insert movement instead of being repeatedly concentrated on one fixed contact point. In addition, the insert is shaped to match the curvature of the femoral component closely, which helps spread load across a wider surface during weight bearing. Compared to older fixed bearing designs, this approach aims to reduce insert wear and support longer term fixation in the treated compartment.
Partial knee replacement is still surgery, so it carries risks such as infection, blood clots, stiffness, bleeding, and implant related issues like loosening or wear over time. Beyond these general risks, the main limitation is that only one compartment is treated. Should arthritis progress in other parts of the knee later on, symptoms can return even if the replaced compartment is doing well. When that happens, further treatment might be needed, including the conversion to a total knee replacement in some cases.
In the early stages of recovery, your orthopaedics specialist will ask you to avoid activities that place heavy impact, twisting, or sudden load through the knee. This includes movements that involve running, jumping, or quick pivots. Since your knee is still regaining stability and confidence, it’s also sensible to be more cautious on uneven ground or in situations where a fall is likely to happen. Instead, activity is gradually built through physiotherapy, with progression guided by how steady and comfortable your movement feels.
As recovery speed differs from person to person, timelines are best treated as a guide rather than a promise. Still, most recovery follows a familiar pattern. In the early weeks, the focus is on the reduction of swelling and pain in order for your walks to feel steadier again. Once your knee is moving more comfortably, physiotherapy then shifts towards the rebuilding of strength and control, which often takes several more weeks. As daily movement becomes easier for you, walking distance and routine tasks are then increased in a progressive manner as opposed to the return to full load all at once. However, full recovery will take months, especially if you’re returning to longer distances, heavier work demands, or sport specific movements.
Our friendly team is here to serve you. For urgent enquiries and appointment requests, please call or WhatsApp us directly.
