It starts with your big toe no longer pointing straight. As it begins angling towards the second toe, a small bump forms at the base of the first metatarsophalangeal (MTP) joint, which is the “knuckle” where the toe meets the foot. At first, it can still feel manageable, even if the toe already looks different. However, as the joint keeps taking load over time, discomfort or pain starts to occur more frequently, and soon it becomes harder to ignore what’s happening in your foot.
And as the toe angle increases and the bump becomes more prominent, footwear can begin pressing more on one side. At the same time, the front of the foot starts taking weight less cleanly, and walking can feel less comfortable over time. With these changes in shape and load, the next step is understanding the pattern your bunion is following, and the stage the joint is already in.

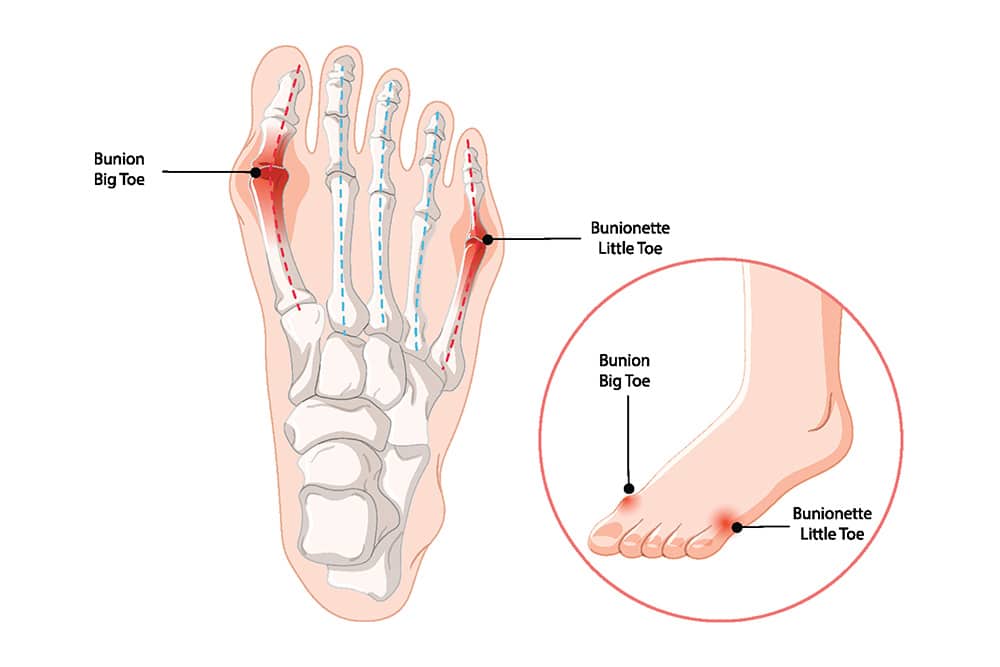
A bunion is also known as hallux valgus, a condition that develops when the big toe begins angling towards the second toe and the joint at its base becomes more prominent. However, a similar bump can also develop at the base of the little toe (the fifth MTP), which is known as a bunionette or Tailor’s Bunion. So, before you decide on the most appropriate treatment option, it helps to know which type you are dealing with, and how far it has progressed.
This is the most common type of bunion, where the bump forms at the base of the big toe and becomes more prominent as the toe angle increases.
A bunionette forms at the base of the little toe, on the outer side of the forefoot. In many cases, it becomes noticeable when footwear pressure or repeated rubbing irritates the joint area over time. As the bump becomes more prominent, pain and inflammation can start showing up more often, especially in snug shoes.
Because bunions and bunionettes affect toe alignment and how pressure moves through the forefoot, symptoms often show up during walking, in tighter footwear, or when the joint starts feeling stiffer under load. Common ones include:


There is rarely one single reason a bunion develops. In many cases, it forms when the foot is predisposed to toe misalignment, then daily pressure and footwear pressure gradually push the joint further out of position over time. This is why bunions are often linked to a combination of inherited structure, movement mechanics, and ongoing strain through the forefoot. Common causes include:
Diagnosis usually begins with a specialist assessment to determine whether your pain is coming from a bunion related alignment issue at the toe joint, or whether it’s another joint problem such as gout (podagra). Because bunion and gout symptoms can overlap, the evaluation focuses on toe alignment, joint movement, and pain response under load, with imaging used to confirm severity and guide treatment decisions. In Singapore, the following methods are commonly used to diagnose bunions:

Treatment is guided by how much the bunion is affecting your choice of footwear and daily movement, along with how far alignment has shifted on assessment. An orthopaedic specialist will first look at how the joint is coping under load and how far the deformity has progressed. In most cases, the discussion is then centred on timing, because the stage of the bunion often determines which approach is more appropriate.
At an intermediate stage, minimally invasive bunion correction is often more suitable, with a recovery timeline that feels more manageable. As severity increases, minimally invasive techniques are less suitable, and open surgery becomes the more common option. Either way, treatment usually starts with steps that reduce irritation and improve walking comfort, before surgery is considered.
For milder bunions, early symptoms, or cases where pain is still manageable, non-surgical care can help reduce irritation and improve comfort. More specifically, the goal is to reduce joint pressure and keep walking more comfortable, especially when footwear is triggering symptoms.
When symptoms keep recurring despite non-surgical care, or when toe alignment has shifted far enough to limit function, minimally invasive surgery (MIS) for correcting bunions can be considered. This is an advanced surgical procedure, and in selected cases it can also address hammer toes. At the centre of this approach is precise bone alignment and joint realignment, while keeping soft tissue disruption to a minimum.
When deformity becomes severe, the toe can drift further out of alignment and daily walking can start feeling less comfortable over time. In these cases, open surgery is more commonly considered, especially when a wider correction approach is needed to restore stability and function through the foot.
Note: Bunion surgery is usually not done for cosmetic concerns alone because bunions involve bone and joint misalignment. This is also why simply shaving the bony prominence rarely solves the underlying problem, and is usually only considered as part of a wider correction plan.
Bunions don’t always need immediate medical treatment, especially if there is only mild discomfort and daily movement still feels manageable. However, once symptoms start interfering more often, or footwear choice becomes increasingly limited, it helps to have the joint checked before the problem worsens further.
As pain becomes more persistent, a specialist review helps confirm whether the bunion is progressing and whether walking comfort and daily function are starting to be affected. It’s worth getting checked when:
At this stage, the next step becomes clearer, whether your symptoms can stay controlled without surgery, or whether correction should be considered for your bunions.


Once bunion symptoms start recurring more often, everyday routines start getting adjusted around discomfort. Footwear gets chosen based on what feels tolerable instead of preference and functionality, steps get shortened without you realising it, and daily movement starts getting paced around flare ups. Over time, these small adjustments can add up, especially when discomfort starts lingering longer or flaring more easily with everyday walking. And because bunions involve bone and joint alignment, the deformity can still progress despite your efforts to adapt around it. As a result, the cost of delay is that the deformity can become more severe, which makes correction more complex and can reduce the suitability of minimally invasive techniques.
And because change is gradual, a proper review helps bring clarity to what’s happening through the joint and alignment, and what can be improved. At Oxford Orthopaedics, care follows established orthopaedic practice and treatment pathways commonly used in Singapore. Our specialists will first review findings in detail and then explain how they relate to your symptoms, movement demands, and longer-term function. Next, the best options are discussed, whether symptoms can stay controlled with non-surgical care or whether surgery should be considered. To speak to a specialist, please contact the clinic to arrange for a consultation.
A bunion happens when the big toe gradually drifts toward the second toe and the joint at its base becomes more prominent. As alignment shifts, the bump can enlarge, and shoes often start pressing against the side of the forefoot. A similar deformity can also form at the little toe joint, which is called a bunionette. Although the bump is what you notice first, the underlying issue is bone and joint misalignment that continues shifting under everyday load.
Bunions develop when the forefoot is predisposed to misalignment, then everyday load gradually shifts the big toe joint further out of position. Genetics plays a major role, especially if a parent has bunions or related foot mechanics issues. Over time, joint laxity, tendon imbalance, and movement patterns add strain during push off, which can be amplified when calf tightness increases forefoot loading. Tight footwear and narrow toe boxes can worsen irritation by crowding the toes, but they are rarely the only underlying cause. In some cases, inflammatory joint conditions such as RA or lupus can also contribute to swelling and pain around the joint.
Bunions and gout can both cause pain and swelling around the big toe joint, which is why they are often confused. The difference is the cause. A bunion is a structural alignment problem that develops gradually, while gout is an inflammatory flare triggered by uric acid crystals inside the joint. Because symptoms can overlap, a proper assessment by an orthopaedic specialist can help confirm the diagnosis, by checking toe alignment, joint movement, and pain response under load, with imaging or further testing implemented when needed.
Bunions often worsen over time because the joint continues taking load while the toe remains out of alignment. As the deformity progresses, pain can become more frequent, and finding shoes that fit comfortably can become more difficult. In more severe cases, the big toe can crowd the smaller toes, increasing pressure through the forefoot and contributing to hammer toe changes over time. A bunionette can also become more symptomatic when rubbing and compression persist along the outer side of the foot, especially in snug footwear.
If a bunion continues progressing, symptoms often shift from occasional irritation to pain that returns more frequently with walking and standing. As pressure patterns change across the forefoot, complications can develop, including bursitis, hammertoe changes, osteoarthritis (OA) changes at the joint, or pain under the ball of the foot (metatarsalgia). Over time, this can limit walking comfort and footwear choice. With an early review by an orthopaedic specialist, you can confirm how far it has shifted, understand what is driving your symptoms, and explore the best options for your foot.
The time it takes to treat bunions will depend on severity and whether non-surgical care is adequate or surgery is required. For milder cases, symptoms often start settling within weeks once footwear pressure is reduced and daily load is managed better. If there’s a need for surgery, recovery will vary because different correction methods involve different levels of realignment. In suitable cases, an MIS approach can support a quicker return to routine activities. In comparison, conventional open surgeries often require a longer recovery period due to the larger soft tissue exposure involved, along with the extra time needed for swelling to settle and the foot to regain daily comfort in footwear.
Bunion surgery is done to correct alignment at the joint, so recurrence is uncommon for most patients once healing is complete. However, a small percentage of patients can still experience recurrence over time, whether the correction was done at the big toe joint or along the outside of the foot for a bunionette. This tends to happen when the underlying drivers remain, such as genetics, foot structure, walking mechanics, and choice of footwear that continue stressing the forefoot over time.
Our friendly team is here to serve you. For urgent enquiries and appointment requests, please call or WhatsApp us directly.
